Best Kidney Transplant Specialists in Artemis Hospital Gurgaon
 30 December,2025
Read More
30 December,2025
Read More
Enquire now in case of any assistance needed
 24 May,2024
24 May,2024

Having a child is a blessing in itself, but having a healthy child makes the event more joyful. In today's world, the prevalence of various diseases has increased. Multiple conditions can be present during birth, and congenital heart disease or defect (CHD) is one of them. It results from disruptions during fetal development, affecting the heart's structure, including chambers, valves, or blood vessels.
Congenital heart defect, being a prevalent congenital disability globally, varies in severity, requiring diverse treatment approaches. According to the World Heart Federation, one out of every 100 children born around the world has CHD. Nearly half of the children with congenital heart disease will require medical intervention at some point in their lifetime, with a quarter needing it within the first year of life for survival.
Early detection of CHD is crucial for effective management, and prenatal screenings contribute to timely intervention. Treatment options, from lifestyle adjustments to surgical procedures, depend on the specific defects.
Fill up the form and get assured assitance within 24 hrs!
Congenital heart disease comprises a range of structural or functional anomalies in the heart present at birth. These abnormalities, often affecting the heart chambers, valves, or blood vessels, result from irregularities during fetal development.
Advancements in surgical techniques and medical technologies have improved outcomes for many individuals with congenital heart defects, allowing them to lead fulfilling lives with appropriate management and care.
Doctors categorize congenital heart diseases into two major subgroups – cyanotic congenital heart diseases (low blood oxygen level) and acyanotic congenital heart diseases (average blood oxygen level).
Cyanotic heart disease results in reduced oxygen delivery to the body. Babies born with cyanotic CHD typically have low oxygen levels and require surgery. Examples of cyanotic congenital heart disease include –
In acyanotic congenital heart diseases, the heart pumps blood with a sufficient amount of oxygen in it. However, the blood is pumped abnormally around the body. Examples of acyanotic congenital heart disease are –
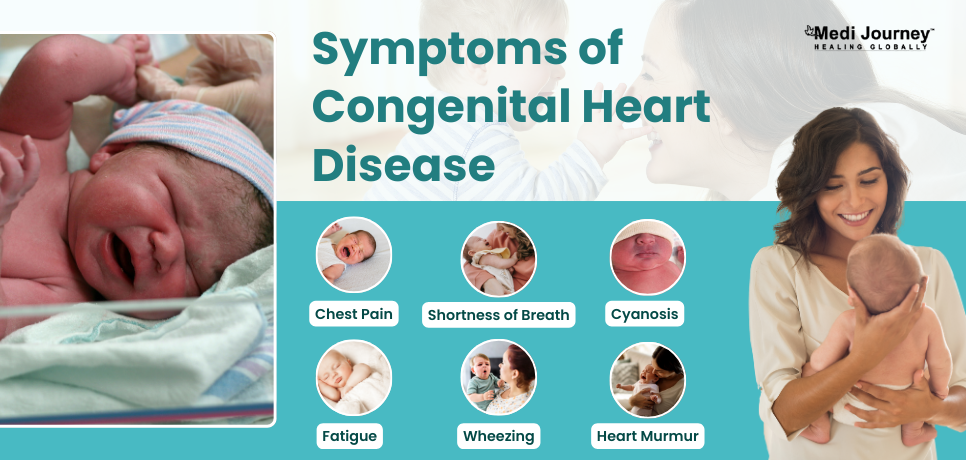
In some cases where the defect is mild, the symptoms of CHD might be vague and difficult to notice till later in life. The symptoms vary greatly depending on the age, number of defects, severity of CHD, and the type of defect.
Common warning signs that congenital heart disease show are –
One must consult an expert pediatric cardiologist if the child is experiencing unexplained chest pain, extreme shortness of breath, or loss of consciousness.
If the pediatric cardiologist suspects a congenital heart defect, they will perform a general physical examination. During physical examination, they will –
Based on the findings of physical examinations, the doctor may further order a few diagnostic tests to confirm the presence of a CHD. Some of the standard tests that help in detecting CHDs are –
It's not possible to always identify the cause of congenital heart defects. Changes in genes, taking certain medications (especially during pregnancy), health conditions, environmental factors, and lifestyle factors such as smoking can all contribute to congenital heart defects.
Researchers have identified various risk factors that can increase the chances of a child being born with a heart defect. These include –
Women who are pregnant or planning to get pregnant in the future can take certain precautions that do not necessarily provide a guarantee against CHD but reduce the risks to a significant extent.
Always have an open discussion with your cardiologist whenever you plan to get pregnant. They can help you have a safe pregnancy and guide you in lowering the risks of congenital heart defects.

Children born with heart defects are always at the risk of developing further problems. Complications of CHD might be present since birth or show up later in adulthood. Common complications associated with congenital heart defects are –
With advancements in medical sciences, the chances of diagnosing and successfully treating congenital heart defects are higher than ever. Several renowned cardiology hospitals have the latest techniques available to perform necessary surgical interventions. However, not everyone with CHD may require treatment, as some mild defects may resolve on their own.
Treatment options for congestive heart disease depend on the severity of the case and the type of the defect. Common modalities available to treat CHD are –
Congenital heart defects are becoming more common. If you plan to get pregnant, it's important to consult a cardiologist to understand the risk factors and ensure a safe pregnancy. Not all children with heart defects require surgery, as some may close on their own. With advancements in medical technology, there are minimally invasive treatments for CHD. It's essential to educate yourself about your child's health issues to make informed choices.
Fill up the form and get assured assitance within 24 hrs!
Doctor of Pharmacy
Dr. Deepanshu Siwach is a skilled clinical pharmacist with a Doctor of Pharmacy degree.?He has 4+?years of experience and has worked with thousands of patients. He has been associated with some of the top hospitals, such as Artemis Gurgaon.
Dr. Aseem Ranjan Srivastava is an experienced Pediatric Cardiothoracic Surgeon specializing in Minimal Access and Robotic Cardiac Surgery. He strongly recommends prompt corrective repair when possible....
Senior Consultant
Medical Oncologist
Nanavati Super Specialty Hospital, Mumbai
WhatsApp UsSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Super Speciality Hospital, Shalimar Bagh, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
WhatsApp UsThe Art of Effective Communication
 30 December,2025
Read More
30 December,2025
Read More
 24 December,2025
Read More
24 December,2025
Read More
 23 December,2025
Read More
23 December,2025
Read More
 17 December,2025
Read More
17 December,2025
Read More
 16 December,2025
Read More
16 December,2025
Read More
 10 December,2025
Read More
10 December,2025
Read More
Trusted by Patients
"I am Asim from Bangladesh and was looking for treatment in India for neuro. I visited many websites to get the complete information regarding the treatment but I was not satisfied as I was getting confused. In the meanwhile, one of my friends suggested I seek help from Medi Journey as he experienced his medical journey very smoothly and was satisfied with it. They have filtered the top 10 doctors as per experience, the success rate of surgery & profile, so it helps us to choose the best treatment in India. "
"For my knee surgery, Medi Journey guided me to BLK Hospital where I received exceptional care. The team's support and the expertise at BLK Hospital exceeded my expectations. Thank you Medi Journey for making my medical journey stress-free. "
"I came from Iraq for my granddaughter's eye surgery in India facilitated by Medi Journey, due to critical cases they advised us to get a second opinion from the different hospitals before going to surgery. Finally, we went to Fortis Escort Hospital, which helped us to get more confidence for diagnosis. Fortis Escort Hospital has the best eye surgeon team with the latest instruments. Thanks to all team members for providing a high-quality treatment in India at an affordable cost. "
"I came for my hair transplant in India, before coming I was so confused about choosing the best clinic and surgeon for me. But thanks to God one of my friends had a hair transplant in India through Medi Journey. He recommended me to go with them. I am completely happy with my experience with them. They were always very fast in their responses to me. the success rate of my hair transplant surgery is 100%."
"Artemis Hospital, suggested by Medi Journey, turned out to be a great choice for my treatment. The personalized assistance and medical care were exceptional. I'm grateful to Medi Journey for guiding me to a hospital that perfectly matched my needs. Highly recommended! "
"I came from Afghanistan for my treatment in India at Jaypee Hospital, Noida. I had a fantastic experience with Medi Journey. Kudos to them for their incredible support during my medical journey. They not only took care of all the logistics but also connected me with a fantastic healthcare team. Efficient, caring, and highly recommended for a hassle-free medical tourism experience."
"I am Adam from Kano, Nigeria, one of my friends from Nigeria was facilitated by Medi Journey, and he recommended us to go with them. I sent my all reports to them and within 48 hours they reverted with 4 options from different hospitals. They helped me to get a Visa letter from the hospital, arrange pick-up from the airport, and book a hotel for me. Their team is very honest and throughout our stay in India they are with us they are caring for us like his family members. BLK Hospital is the best hospital in India with a top surgical oncologist surgeon team, a very advanced OT, and a Radiotherapy department. I wish more success to Medi Journey. "
"Great experience at the Max Hospital for my spine surgery and was successfully done. I thank my neurosurgeon and his entire team. I recommended all of my country's people to Medi Journey for treatment in India, they choose the best hospital, the best doctors, and the best cost for patients."
"I came to India from Dhaka, Bangladesh for my father-in-law's cardiac surgery at Fortis Hospital. I was confused about choosing the best surgeon for him before coming, but their team helped me to choose the best hospital and best cardiac surgeon in India with very good cost and 100% success rate of surgery. I am very happy with the services, really they make my journey so comfortable that make me feel at home. Thanks again and I like people to choose "Medi Journey" as your travel guide. "
"I am Mohammad from Bangladesh came to India for my general health checkup. Medi Journey offers me the complete package including Pick-up from the airport, hotel services, and 24-hour assistance. They guide you to choose the best hospital in India, the best cost of treatment with top-most doctors and give you complete information about hotel booking, and pick-up from the airport before coming to India They have the best team to help. Always choose Medi Journey for your treatment in India."