Ghana Patient Successfully Treated With Minimally Invasive Shoulder Surgery in India
 26 November,2024
Read More
26 November,2024
Read More
Enquire now in case of any assistance needed
The human heart is one of the most important organs that never rests. But what happens when this vital organ gets diseased beyond repair? For thousands of individuals, a heart transplant becomes their only hope for survival. A heart transplant is a miracle of modern medicine—a chance at life for those with severe heart diseases. Let's explore this incredible procedure in detail, unraveling everything from donor eligibility to recovery.
A heart transplantation is a complex surgical procedure that replaces a failing or diseased heart with a healthy heart from a deceased donor. The goal is to restore proper blood circulation, ensuring oxygen reaches every cell in the body.
Why is it needed? For some patients, medication, lifestyle changes, or even less invasive surgeries can't halt the progression of their condition. Without a new heart, their quality of life diminishes, and survival becomes uncertain. The idea of taking one person's heart and giving it to another might seem like something out of science fiction. Yet, it has become a routine practice in leading medical centers worldwide, saving lives every day.
The history of heart transplantation is nothing short of inspiring. Dr. Christiaan Barnard and his team performed the first successful human heart transplant on 3rd December 1967, in Cape Town, South Africa. The recipient, Louis Washkansky, was a 53-year-old man suffering from severe heart disease. Although he survived only 18 days due to complications, the procedure proved that heart transplantation was possible. Since then, advances in surgical techniques, medications to prevent rejection, and better patient care have made heart transplants more successful and routine.
Heart transplants are more common than you might think, but they remain a specialized procedure. Globally, about 5,000 heart transplants are performed annually. In the United States alone, around 3,500 such surgeries occur annually. Yet, the number of people waiting for a donor heart (over 50,000) far exceeds the availability of suitable organs.
Why is the availability so limited? The answer lies in the complexity of matching donors with recipients and the scarcity of eligible donors.
Organ donation is an act of unparalleled generosity. However, only some are eligible to donate their heart. Criteria for donating a heart are:
To become a heart donor, you must register with your national organ donor register.
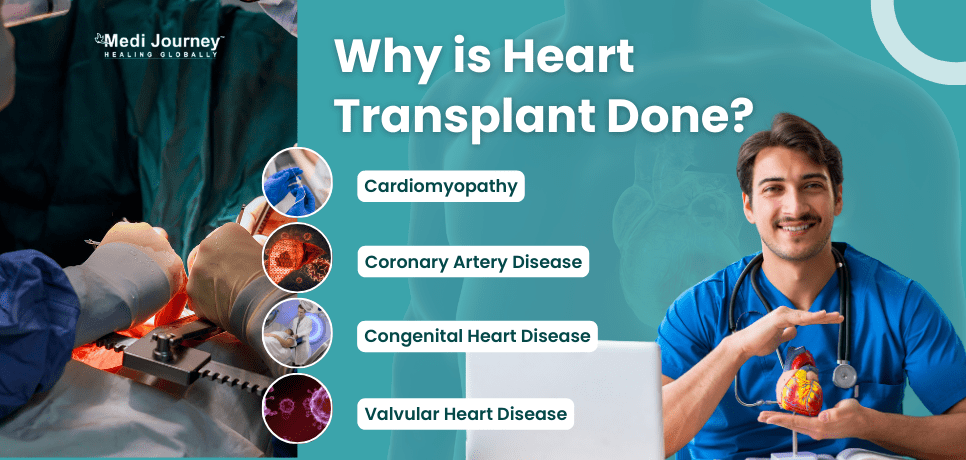
A heart transplant is not the first solution doctors turn to when treating heart conditions. It's usually a last resort when other treatments have failed. Common conditions leading to heart transplantation are:
Imagine struggling every day to breathe or feeling fatigued after the simplest tasks. For many, a heart transplant offers the chance to regain a normal, active life.
The journey to a heart transplant is rigorous. It involves several steps to ensure the best outcomes.
How are priorities set? Allocation depends on factors like medical urgency, blood type compatibility, and time spent on the list.
A heart transplant is an intricate procedure that demands precision and expertise. It involves the following steps.
The surgery usually lasts 4–6 hours. Would you believe that this life-saving procedure hinges on a critical 4–6 hour window in which the donor heart must remain viable?
Recovery after a heart transplant is a long and carefully monitored process.
Full recovery can take six months to a year. Imagine the patience and discipline it requires to adjust to this new chapter of life.
Like any major medical procedure, heart transplants come with both benefits and risks. Advantages of heart transplant include:
Heart transplants today are safer than ever, thanks to improved surgical techniques and medications. The survival rate is encouraging. About 85-90% of recipients survive the first year post-transplant, and many go on to live 10–15 years or longer. However, the procedure is not without risks. Surgeons and medical teams work tirelessly to minimize complications and ensure the best possible outcomes.
Yes, heart transplants are possible—and often necessary—for children with severe congenital heart defects or heart failure. Finding a suitable donor for children is particularly challenging due to the need for size compatibility. Pediatric heart transplants require even greater precision and care, but the results are often life-changing. Success rates are also better in pediatric heart transplants, with over 90% of children surviving one year after the transplant and ~70% living after 10 years of transplantation.
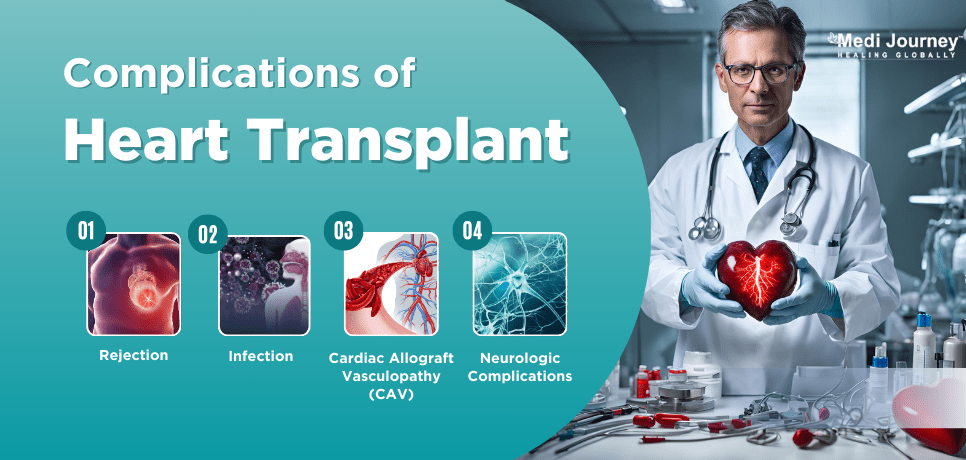
Heart transplants are not without risks. Understanding potential complications helps patients and families prepare. Common complications and risks associated with heart transplants are:
Alcohol consumption should not be encouraged after a heart transplant. It has several negative impacts on the body and has no nutritional value. However, if one cannot completely abstain from alcohol, moderate consumption (not more than one drink a day) can be allowed, but it's essential to consult your doctor.
Vaccines are critical for preventing infections, and there are certain vaccines that you can receive after a heart transplant. The flu vaccine is one such example. However, vaccines containing live viruses are generally not recommended due to the weakened immune system.
Post-transplant life involves adjustments, but most recipients can enjoy a relatively normal lifestyle. Always follow your healthcare provider's advice to balance safety and quality of life.
Sometimes, the transplanted heart may fail due to rejection, infection, or other issues. In such cases, retransplantation may be considered. Recently, Karnataka witnessed its first heart retransplant, where Prof. Dr. Nagamalesh U M performed the second heart transplant on a 32-year-old engineer.
A heart transplant is not just a medical procedure. For recipients, it's a chance to live again. For donors and their families, it's an opportunity to give the ultimate gift of life. Modern medicine continues to push the extremities of what is achievable, turning once-impossible dreams into everyday miracles. Heart transplantation is a testament to human ingenuity and kindness—a reminder of what we can achieve together. Could you become an organ donor and save a life?
Doctor of Pharmacy
Dr. Deepanshu Siwach is a skilled clinical pharmacist with a Doctor of Pharmacy degree. He has 4+ years of experience and has worked with thousands of patients. He has been associated with some of the top hospitals, such as Artemis Gurgaon.
Dr. Aseem Ranjan Srivastava is an experienced Pediatric Cardiothoracic Surgeon specializing in Minimal Access and Robotic Cardiac Surgery. He strongly recommends prompt corrective repair when possible....
Senior Consultant
Medical Oncologist
Nanavati-Max Super Speciality Hospital, Mumbai
Book an Appointment Talk To ExpertSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Super Speciality Hospital, Shalimar Bagh, New Delhi
Book an Appointment Talk To ExpertSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Smart Super Speciality Hospital, Saket, New Delhi
Book an Appointment Talk To ExpertSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
Book an Appointment Talk To ExpertSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
Book an Appointment Talk To ExpertSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
Book an Appointment Talk To ExpertFill up the form and get assured assitance within 24 hrs!
The Art of Effective Communication
 25 November,2024
Read More
25 November,2024
Read More
 05 November,2024
Read More
05 November,2024
Read More
Trusted by Patients
"I am Asim from Bangladesh and was looking for treatment in India for neuro. I visited many websites to get the complete information regarding the treatment but I was not satisfied as I was getting confused. In the meanwhile, one of my friends suggested I seek help from Medi Journey as he experienced his medical journey very smoothly and was satisfied with it. They have filtered the top 10 doctors as per experience, the success rate of surgery & profile, so it helps us to choose the best treatment in India. "
"For my knee surgery, Medi Journey guided me to BLK Hospital where I received exceptional care. The team's support and the expertise at BLK Hospital exceeded my expectations. Thank you Medi Journey for making my medical journey stress-free. "
"I came from Iraq for my granddaughter's eye surgery in India facilitated by Medi Journey, due to critical cases they advised us to get a second opinion from the different hospitals before going to surgery. Finally, we went to Fortis Escort Hospital, which helped us to get more confidence for diagnosis. Fortis Escort Hospital has the best eye surgeon team with the latest instruments. Thanks to all team members for providing a high-quality treatment in India at an affordable cost. "
"I came for my hair transplant in India, before coming I was so confused about choosing the best clinic and surgeon for me. But thanks to God one of my friends had a hair transplant in India through Medi Journey. He recommended me to go with them. I am completely happy with my experience with them. They were always very fast in their responses to me. the success rate of my hair transplant surgery is 100%."
"Artemis Hospital, suggested by Medi Journey, turned out to be a great choice for my treatment. The personalized assistance and medical care were exceptional. I'm grateful to Medi Journey for guiding me to a hospital that perfectly matched my needs. Highly recommended! "
"I came from Afghanistan for my treatment in India at Jaypee Hospital, Noida. I had a fantastic experience with Medi Journey. Kudos to them for their incredible support during my medical journey. They not only took care of all the logistics but also connected me with a fantastic healthcare team. Efficient, caring, and highly recommended for a hassle-free medical tourism experience."
"I am Adam from Kano, Nigeria, one of my friends from Nigeria was facilitated by Medi Journey, and he recommended us to go with them. I sent my all reports to them and within 48 hours they reverted with 4 options from different hospitals. They helped me to get a Visa letter from the hospital, arrange pick-up from the airport, and book a hotel for me. Their team is very honest and throughout our stay in India they are with us they are caring for us like his family members. BLK Hospital is the best hospital in India with a top surgical oncologist surgeon team, a very advanced OT, and a Radiotherapy department. I wish more success to Medi Journey. "
"Great experience at the Max Hospital for my spine surgery and was successfully done. I thank my neurosurgeon and his entire team. I recommended all of my country's people to Medi Journey for treatment in India, they choose the best hospital, the best doctors, and the best cost for patients."
"I came to India from Dhaka, Bangladesh for my father-in-law's cardiac surgery at Fortis Hospital. I was confused about choosing the best surgeon for him before coming, but their team helped me to choose the best hospital and best cardiac surgeon in India with very good cost and 100% success rate of surgery. I am very happy with the services, really they make my journey so comfortable that make me feel at home. Thanks again and I like people to choose "Medi Journey" as your travel guide. "
"I am Mohammad from Bangladesh came to India for my general health checkup. Medi Journey offers me the complete package including Pick-up from the airport, hotel services, and 24-hour assistance. They guide you to choose the best hospital in India, the best cost of treatment with top-most doctors and give you complete information about hotel booking, and pick-up from the airport before coming to India They have the best team to help. Always choose Medi Journey for your treatment in India."