Yemeni Patients Choose India for Medical Treatment
 23 December,2024
Read More
23 December,2024
Read More
Enquire now in case of any assistance needed
 15 April,2024
15 April,2024

Pacemaker implantation is a standard medical procedure for treating individuals with abnormal heart rhythms or arrhythmias. Studies reveal over 60% of sudden cardiac arrests are due to irregular heartbeats.
Pacemakers can prevent 1 to 2 million annual deaths worldwide. The procedure involves placing a small device into the chest to help regulate and stabilize the heart's electrical signals.Â
Understanding the different aspects of pacemaker implantation can be crucial for patients and their healthcare providers. This blog aims to shed light on what a pacemaker is, how it works, the benefits of pacemaker implantation, and the risks associated with it.
Pacemakers are small, lightweight devices implanted under the skin near the collarbone. They send electrical impulses to the heart to help maintain a regular heart rate. It weighs about 20 to 50 grams and is the size of a matchbox (or even smaller)!
Pacemaker consists of two parts.
Cardiologists can program pacemakers according to the patient's needs. If the heart skips a beat or beats slowly, the pacemaker can identify it and steadily send electrical signals. If the heart beats normally, the pacemaker won't send any signals.
Several types of pacemakers are available, each designed to cater to specific needs. The three main types are –
Pacemakers also vary in their features and capabilities. Some pacemakers have programmable settings to adjust the pacing rate according to a person's needs. In contrast, others have advanced sensors that can detect changes in a person's activity level to optimize heart rate response.Â
In addition to the main types mentioned, leadless pacemakers are implanted directly into the heart without the need for leads. These devices are smaller in size and reduce the risk of lead-related complications. Leadless pacemakers are particularly beneficial for patients at a higher risk of infection or with limited vascular access to traditional pacemaker placement.

Diseases and disorders that cause abnormal heart rhythms lead to improper blood supply to the body. It is due to the inadequate amount of blood pumped by the heart. Pacemaker implantations help in rectifying such diseases. Some common heart conditions treatable by pacemaker include –
Whether a patient needs a pacemaker is based on thoroughly evaluating their medical history, symptoms, and diagnostic test results. Pacemaker implantation is indicated for individuals with certain heart conditions or abnormal heart rhythms. These include –
Additionally, doctors may recommend pacemakers for individuals at risk of sudden cardiac arrest or for those who have undergone heart surgery and require temporary pacing support during the recovery period.Â
Please note that these symptoms can also indicate other disorders requiring different treatments. Consulting a skilled cardiologist is vital to establishing whether you are the right candidate for pacemaker implantation.
After pacemaker implantation, patients receive comprehensive post-operative care instructions from their healthcare providers. Following these guidelines is essential to promoting proper healing and optimizing the pacemaker's functioning.

Pacemakers help improve patients' quality of life and prevent complications arising from heart rhythm problems. Benefits of pacemaker implantation include –Â
However, pacemaker implantation has potential risks and complications like any medical procedure. These can include –
If you have a pacemaker, you may wonder how to use everyday devices safely. As discussed earlier, pacemaker implantation is a safe procedure. However, you must take a few precautions since it is a battery-operated device. Here are some tips to help you avoid any problems:
In conclusion, understanding pacemaker implantation is crucial for individuals with certain heart conditions or abnormal heart rhythms. Knowing the types of pacemakers available, the indications for implantation, the success rates, and the procedure itself can help patients make informed decisions about their healthcare. Ongoing advancements in pacemaker technology also promise improved treatment options in the future. Consultation with healthcare providers is essential to address specific concerns and ensure the best possible outcomes for pacemaker patients.
Doctor of Pharmacy
Dr. Deepanshu Siwach is a skilled clinical pharmacist with a Doctor of Pharmacy degree. He has 4+ years of experience and has worked with thousands of patients. He has been associated with some of the top hospitals, such as Artemis Gurgaon.
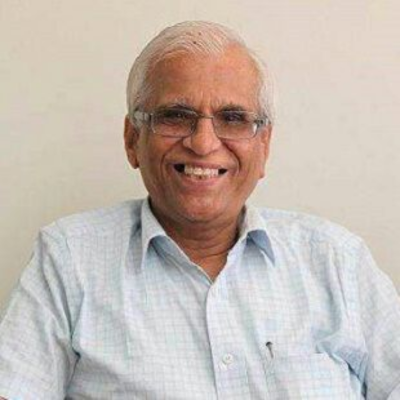
Chairman
Cardiac Electrophysiologist, Interventional Cardiologist
Dr. T. S. Kler is a Padma Bhushan recipient with over 48 years of experience as an Interventional Cardiologist and Electrophysiologist. He has performed over 35,000 angioplasties and is a pioneer in electrophysiology, having established the first department in India. ...
Senior Consultant
Medical Oncologist
Nanavati-Max Super Speciality Hospital, Mumbai
Book an Appointment Talk To ExpertSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Super Speciality Hospital, Shalimar Bagh, New Delhi
Book an Appointment Talk To ExpertSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Smart Super Speciality Hospital, Saket, New Delhi
Book an Appointment Talk To ExpertSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
Book an Appointment Talk To ExpertSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
Book an Appointment Talk To ExpertSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
Book an Appointment Talk To ExpertFill up the form and get assured assitance within 24 hrs!
The Art of Effective Communication
 23 December,2024
Read More
23 December,2024
Read More
 10 December,2024
Read More
10 December,2024
Read More
 05 December,2024
Read More
05 December,2024
Read More
 04 December,2024
Read More
04 December,2024
Read More
 02 December,2024
Read More
02 December,2024
Read More
 27 November,2024
Read More
27 November,2024
Read More
Trusted by Patients
"I am Asim from Bangladesh and was looking for treatment in India for neuro. I visited many websites to get the complete information regarding the treatment but I was not satisfied as I was getting confused. In the meanwhile, one of my friends suggested I seek help from Medi Journey as he experienced his medical journey very smoothly and was satisfied with it. They have filtered the top 10 doctors as per experience, the success rate of surgery & profile, so it helps us to choose the best treatment in India. "
"For my knee surgery, Medi Journey guided me to BLK Hospital where I received exceptional care. The team's support and the expertise at BLK Hospital exceeded my expectations. Thank you Medi Journey for making my medical journey stress-free. "
"I came from Iraq for my granddaughter's eye surgery in India facilitated by Medi Journey, due to critical cases they advised us to get a second opinion from the different hospitals before going to surgery. Finally, we went to Fortis Escort Hospital, which helped us to get more confidence for diagnosis. Fortis Escort Hospital has the best eye surgeon team with the latest instruments. Thanks to all team members for providing a high-quality treatment in India at an affordable cost. "
"I came for my hair transplant in India, before coming I was so confused about choosing the best clinic and surgeon for me. But thanks to God one of my friends had a hair transplant in India through Medi Journey. He recommended me to go with them. I am completely happy with my experience with them. They were always very fast in their responses to me. the success rate of my hair transplant surgery is 100%."
"Artemis Hospital, suggested by Medi Journey, turned out to be a great choice for my treatment. The personalized assistance and medical care were exceptional. I'm grateful to Medi Journey for guiding me to a hospital that perfectly matched my needs. Highly recommended! "
"I came from Afghanistan for my treatment in India at Jaypee Hospital, Noida. I had a fantastic experience with Medi Journey. Kudos to them for their incredible support during my medical journey. They not only took care of all the logistics but also connected me with a fantastic healthcare team. Efficient, caring, and highly recommended for a hassle-free medical tourism experience."
"I am Adam from Kano, Nigeria, one of my friends from Nigeria was facilitated by Medi Journey, and he recommended us to go with them. I sent my all reports to them and within 48 hours they reverted with 4 options from different hospitals. They helped me to get a Visa letter from the hospital, arrange pick-up from the airport, and book a hotel for me. Their team is very honest and throughout our stay in India they are with us they are caring for us like his family members. BLK Hospital is the best hospital in India with a top surgical oncologist surgeon team, a very advanced OT, and a Radiotherapy department. I wish more success to Medi Journey. "
"Great experience at the Max Hospital for my spine surgery and was successfully done. I thank my neurosurgeon and his entire team. I recommended all of my country's people to Medi Journey for treatment in India, they choose the best hospital, the best doctors, and the best cost for patients."
"I came to India from Dhaka, Bangladesh for my father-in-law's cardiac surgery at Fortis Hospital. I was confused about choosing the best surgeon for him before coming, but their team helped me to choose the best hospital and best cardiac surgeon in India with very good cost and 100% success rate of surgery. I am very happy with the services, really they make my journey so comfortable that make me feel at home. Thanks again and I like people to choose "Medi Journey" as your travel guide. "
"I am Mohammad from Bangladesh came to India for my general health checkup. Medi Journey offers me the complete package including Pick-up from the airport, hotel services, and 24-hour assistance. They guide you to choose the best hospital in India, the best cost of treatment with top-most doctors and give you complete information about hotel booking, and pick-up from the airport before coming to India They have the best team to help. Always choose Medi Journey for your treatment in India."