The Role of Government Initiatives in Promoting Medical Tourism in India
 02 April,2025
Read More
02 April,2025
Read More
Enquire now in case of any assistance needed
 28 March,2024
28 March,2024
Ventricular septal defect (VSD) is a heart ailment that has been present since birth. It is marked by an opening between the walls separating the heart's lower chambers (ventricles). Approximately 90% of VSDs resolve on their own during childhood.
Treatment options for VSD that do not close on their own depend on the size and severity of the defect. Sometimes, the cardiologist may prescribe medication to manage symptoms and control blood pressure. However, if the defect is large and causes significant symptoms or complications, surgical intervention may be necessary to repair the hole in the septum.
Fortunately, advances in cardiac science have significantly improved the outcomes for individuals with a ventricular septal defect. With proper diagnosis, timely intervention, and ongoing medical care, VSD patients can lead fulfilling lives and enjoy good heart health.
Ventricular Septal Defect (VSD) is one of the most common congenital (birth) heart defects, affecting approximately 1 in 500 births. The heart comprises four chambers: the right atrium, left atrium, right ventricle, and left ventricle. The right and left ventricles have a wall separating them, known as the ventricular septum. VSDs are openings or holes in the ventricular septum, which leads to the blood mixing between both chambers.
The severity of a VSD depends on various factors, such as the location and size of the defect. Small VSDs may close on their own or cause minimal symptoms, while larger defects can lead to significant complications.
One potential complication of VSD is the development of pulmonary hypertension. When blood from the left ventricle flows into the right ventricle through the hole, excessive blood is sent to the lungs. In the long run, this increased blood flow leads to high blood pressure in the lungs, causing strain on the heart.
Based on the location and structure of the ventricular septal defect, VSDs are of 4 significant types.
Ventricular septal defects can range from small to large. The effect of VSD on the body is determined by its size.

Ventricular Septal Defect (VSD) is a condition that can display various symptoms depending on the size and location of the defect. Individuals with small VSDs may not experience symptoms in some cases, while those with more significant defects may exhibit noticeable signs.
Common symptoms of VSD in infants include:
These symptoms occur because the hole in the septum allows blood to flow between the chambers, causing the heart to work harder to pump oxygenated blood throughout the body.
As children with VSD grow older, they may develop symptoms such as:
Ventricular Septal Defect (VSD) is a congenital heart defect characterized by a septum hole separating the heart's two lower chambers. While the exact cause of VSD is unknown, multiple factors play a role in its development.
It is important to note that while these factors may increase the likelihood of VSD, not everyone with these risk factors will have the defect. Furthermore, VSD can also occur in individuals with no known risk factors. Therefore, consulting with a healthcare professional for accurate information and guidance is crucial.
To diagnose VSD, a healthcare professional will typically perform a physical examination, listen for abnormal heart sounds (murmurs), and order additional tests such as an echocardiogram or cardiac catheterization. These tests provide detailed images of the heart, allowing the cardiologists to assess the size and severity of the defect.
It is essential to diagnose and treat VSD early, as this condition can lead to complications such as heart failure, elevated blood pressure in the lungs, or infective endocarditis. With prompt medical intervention, individuals with VSD can often lead normal and healthy lives.
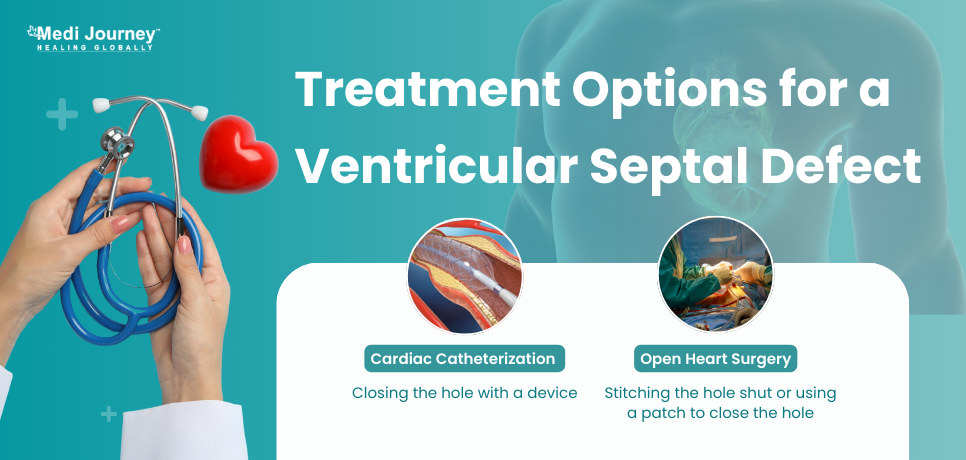
Treatment options for VSD depend on the size and severity of the defect. Small VSDs may sometimes close on their own as the child grows. However, larger defects may require surgical intervention to repair the hole in the septum. The specific surgical intervention will depend on the location and complexity of the defect. Surgical options for ventricular septal defect include –
In both surgeries, the heart tissue grows over the patch or the occluding device and becomes part of the ventricular septum.
After surgery, individuals with VSD will require regular follow-up appointments to monitor their heart health. This may include echocardiograms, electrocardiograms, and other tests to ensure that the defect has been successfully repaired and that the heart is functioning correctly.
Ventricular Septal Defect (VSD), or a hole in the heart, is a congenital (birth) defect with an opening between the heart's lower chambers. Individuals with VSD need regular follow-up appointments with a cardiologist to monitor their heart health and promptly address potential issues. Small VSDs may not require treatment, and people can lead normal, healthy lives without restrictions. However, they must be aware of the signs and symptoms of complications, such as fatigue, rapid breathing, poor weight gain, and recurrent respiratory infections, which may indicate further evaluation and intervention.
Doctor of Pharmacy
Dr. Deepanshu Siwach is a skilled clinical pharmacist with a Doctor of Pharmacy degree.?He has 4+?years of experience and has worked with thousands of patients. He has been associated with some of the top hospitals, such as Artemis Gurgaon.
Chairman
Cardiac Electrophysiologist, Interventional Cardiologist
Dr. T. S. Kler is a Padma Bhushan recipient with over 48 years of experience as an Interventional Cardiologist and Electrophysiologist. He has performed over 35,000 angioplasties and is a pioneer in electrophysiology, having established the first department in India. ...
Senior Consultant
Medical Oncologist
Nanavati-Max Super Speciality Hospital, Mumbai
Book Appointment WhatsApp UsSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Super Speciality Hospital, Shalimar Bagh, New Delhi
Book Appointment WhatsApp UsSenior Director
Gynecologist and Obstetrician, IVF Specialist
Max Smart Super Speciality Hospital, Saket, New Delhi
Book Appointment WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
Book Appointment WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
Book Appointment WhatsApp UsSenior Director
Gynecologist and Obstetrician
Max Smart Super Speciality Hospital, Saket, New Delhi
Book Appointment WhatsApp UsFill up the form and get assured assitance within 24 hrs!
The Art of Effective Communication
 24 January,2025
Read More
24 January,2025
Read More
Trusted by Patients
"I am Asim from Bangladesh and was looking for treatment in India for neuro. I visited many websites to get the complete information regarding the treatment but I was not satisfied as I was getting confused. In the meanwhile, one of my friends suggested I seek help from Medi Journey as he experienced his medical journey very smoothly and was satisfied with it. They have filtered the top 10 doctors as per experience, the success rate of surgery & profile, so it helps us to choose the best treatment in India. "
"For my knee surgery, Medi Journey guided me to BLK Hospital where I received exceptional care. The team's support and the expertise at BLK Hospital exceeded my expectations. Thank you Medi Journey for making my medical journey stress-free. "
"I came from Iraq for my granddaughter's eye surgery in India facilitated by Medi Journey, due to critical cases they advised us to get a second opinion from the different hospitals before going to surgery. Finally, we went to Fortis Escort Hospital, which helped us to get more confidence for diagnosis. Fortis Escort Hospital has the best eye surgeon team with the latest instruments. Thanks to all team members for providing a high-quality treatment in India at an affordable cost. "
"I came for my hair transplant in India, before coming I was so confused about choosing the best clinic and surgeon for me. But thanks to God one of my friends had a hair transplant in India through Medi Journey. He recommended me to go with them. I am completely happy with my experience with them. They were always very fast in their responses to me. the success rate of my hair transplant surgery is 100%."
"Artemis Hospital, suggested by Medi Journey, turned out to be a great choice for my treatment. The personalized assistance and medical care were exceptional. I'm grateful to Medi Journey for guiding me to a hospital that perfectly matched my needs. Highly recommended! "
"I came from Afghanistan for my treatment in India at Jaypee Hospital, Noida. I had a fantastic experience with Medi Journey. Kudos to them for their incredible support during my medical journey. They not only took care of all the logistics but also connected me with a fantastic healthcare team. Efficient, caring, and highly recommended for a hassle-free medical tourism experience."
"I am Adam from Kano, Nigeria, one of my friends from Nigeria was facilitated by Medi Journey, and he recommended us to go with them. I sent my all reports to them and within 48 hours they reverted with 4 options from different hospitals. They helped me to get a Visa letter from the hospital, arrange pick-up from the airport, and book a hotel for me. Their team is very honest and throughout our stay in India they are with us they are caring for us like his family members. BLK Hospital is the best hospital in India with a top surgical oncologist surgeon team, a very advanced OT, and a Radiotherapy department. I wish more success to Medi Journey. "
"Great experience at the Max Hospital for my spine surgery and was successfully done. I thank my neurosurgeon and his entire team. I recommended all of my country's people to Medi Journey for treatment in India, they choose the best hospital, the best doctors, and the best cost for patients."
"I came to India from Dhaka, Bangladesh for my father-in-law's cardiac surgery at Fortis Hospital. I was confused about choosing the best surgeon for him before coming, but their team helped me to choose the best hospital and best cardiac surgeon in India with very good cost and 100% success rate of surgery. I am very happy with the services, really they make my journey so comfortable that make me feel at home. Thanks again and I like people to choose "Medi Journey" as your travel guide. "
"I am Mohammad from Bangladesh came to India for my general health checkup. Medi Journey offers me the complete package including Pick-up from the airport, hotel services, and 24-hour assistance. They guide you to choose the best hospital in India, the best cost of treatment with top-most doctors and give you complete information about hotel booking, and pick-up from the airport before coming to India They have the best team to help. Always choose Medi Journey for your treatment in India."